Are Hospitals Ready for the Coronavirus?
Preparing for Hospital overflow UPDATE
Preparing for hospital overflow. Hospital overflow crisis. Right now, hospitals in Spain and Italy have become hopelessly overwhelmed. Healthcare workers are releasing video clips that show coronavirus patients packed onto chairs and lying on floors, waiting for medical attention. Resources are so scarce that patients are lying on jackets and using their own bags as pillows. Healthcare facilities have fewer and fewer options for situating patients that desperately need access to multiple pieces of medical equipment, and as conditions in the United States worsen, these scenes may become all too common. Read our article here.
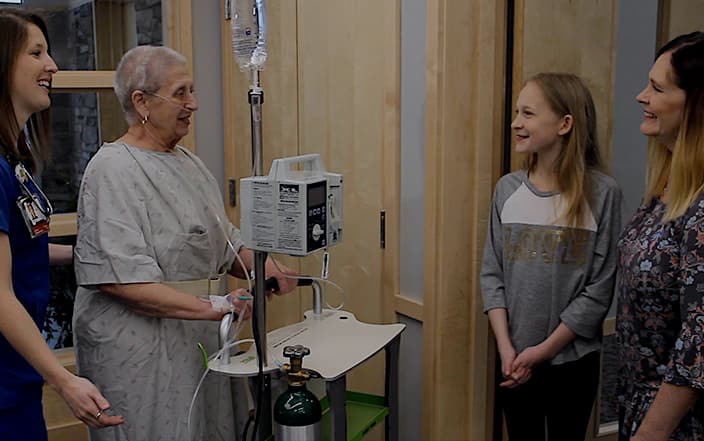
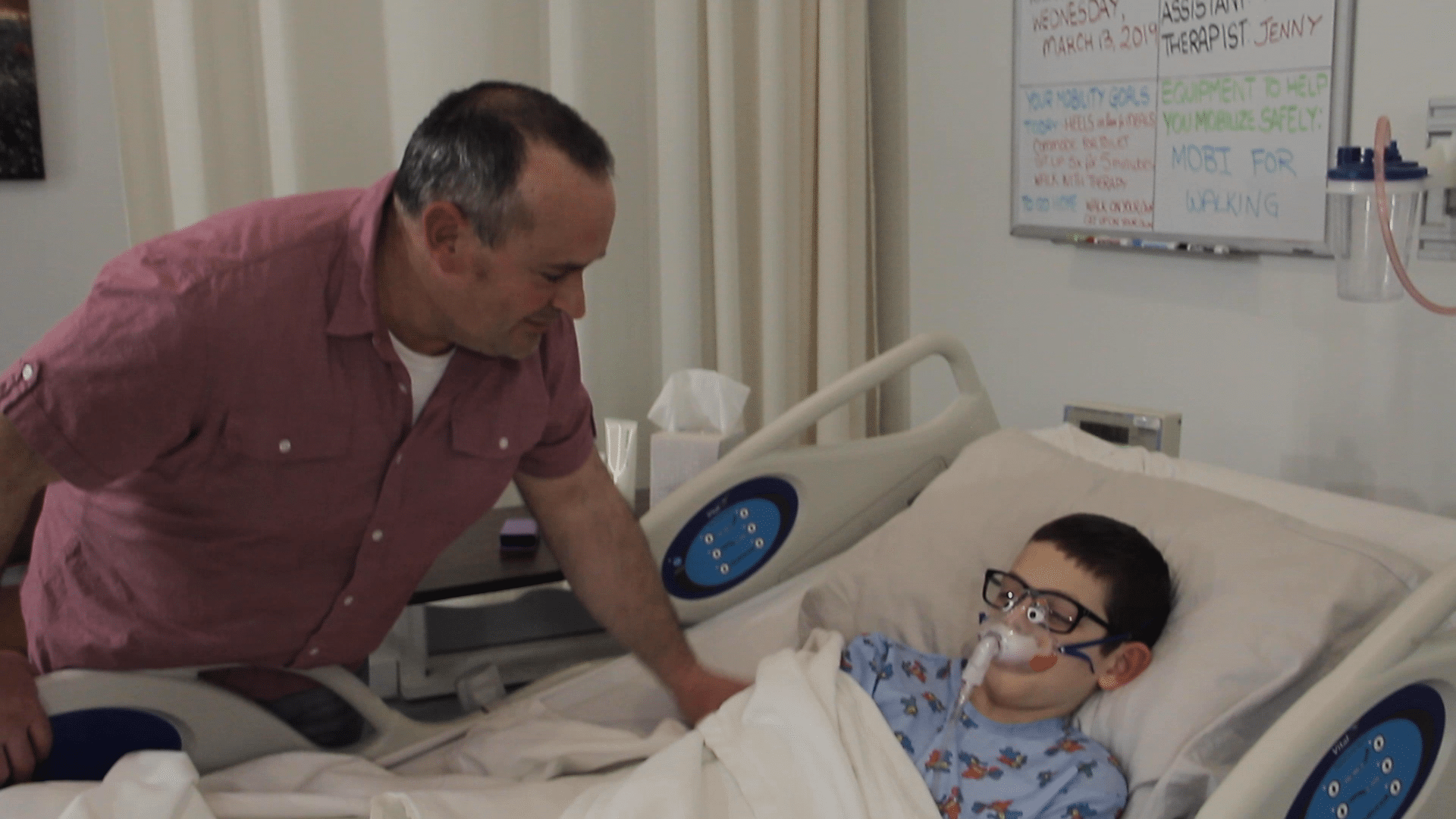
The mobi is a headwall (equipment consolidator) that can be set up in any space that has an electrical outlet: next to a chair, a bed, a cot in the hallway, a cafeteria, or anywhere patients need to be located. The mobi also enables safe early patient mobility improving patient outcomes and decreasing Length of Stay by up to 30%.
See the mobigo here
See the mobilite here
See the mobikidz here
Click here for the full Article