MINIMIZING HOSPITAL-ACQUIRED Complications
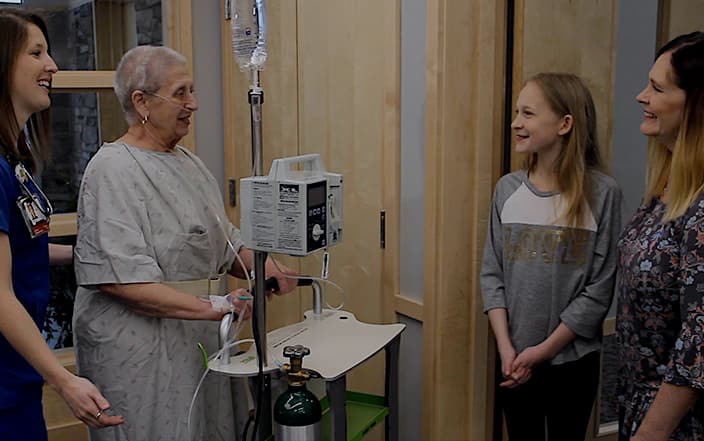
Early Mobilization. Recovering from a major illness or injury can be a slow and difficult process. But when patients are bed-bound, simply being in the hospital can add further complications. In the United States alone, 600,000 patients acquire healthcare-associated infections every year, resulting in nearly 100,000 preventable fatalities (Vaughn 2020). Further complications can include constipation, blood clots, bed sores, delirium, and ICU-acquired weakness, all of which increase the risk of readmission and death. However, early mobilization reduces these risks by activating the body’s own defense mechanisms: improving circulation, decreasing fluid retention, and stimulating the lymphatic, digestive, and nervous systems. Early mobilization keeps patients safe, improves recovery times, and lowers healthcare costs for both the patient and the hospital.
Key Facts:
- A systematic review of medical studies found that early mobilization reduces both costs and the risk of secondary complications. On average, patients who achieved early mobilization experienced two fewer days of delirium, fewer central line and catheter infections, lowered risk of ventilator-assisted pneumonia, and reduced risk of readmission and death. (Hunter 2014)
- For patients who have undergone coronary artery bypass surgery grafting (CABG), mobilization within six hours after surgery significantly reduces the risk of secondary pneumonia. (Strobel 2020)
- An extensive study of patients with traumatic spine injuries revealed that patients who were immobilized for more than 72 hours after surgery were 14% more likely to acquire serious secondary complications (pneumonia, urinary tract infection, deep vein thrombosis, and/or pulmonary embolism). (MacCallum 2020)
- A survey of more than 23,000 lumbar surgery patients showed that mobilization on the day of surgery resulted in a shorter length of stay and significantly decreased risk of bowel obstruction, urinary tract infection, and readmission. (Zakaria 2019)
- For cancer patients who have had part of the lung surgically removed, standard early mobilization (within 24 hours) and physiotherapy is recommended to improve lung volume, clear excess fluid from the lungs, and reduce postoperative pulmonary complications. (Agostini 2020)
- Standardized early mobility protocols can improve outcomes for patients with deep vein thrombosis, decrease length of stay for patients with community-acquired pneumonia, and help elderly patients recovering from major surgery to achieve or maintain independent functionality. (Pashikanti 2012)
Learn more about Livengood Medical Mobi Solutions.