Early Patient Ambulation: What Works Best
Solutions for early patient mobility. As far back as 1949, Dr. D.J. Leithauser wrote that: Ten years ago early ambulation was considered a “crackpot” idea. Today it is recognized and is rapidly approaching a “must” procedure following surgical operation. Seventy years later, Doctors, nurses, and administrators all agree that early patient mobility has tremendously beneficial outcomes, but making sure that early mobility happens requires resources, education, organization, and strategic coordination. How have hospitals and units successfully improved their early patient mobility rates? The simplest answer is to increase staff numbers, but there are a variety of more cost-effective measures that have helped to dramatically improve early mobility outcomes.
Key Facts:
Improve Mobility: Equipment, Patient Awareness, Staff Efficiency, & Hospital Culture
Steps can be taken to improve efficient implementation of early mobility on all four fronts:
EQUIPMENT
- It is important for hospitals to prioritize interventions that allow patient ambulation with less staff involvement. (Murphy 2011)
- The use of an ambulation platform improves the number of ambulation attempts, distance of ambulation, and willingness of patients to attempt ambulation (assisted and unassisted), without increased risk of falls. (Henecke 2015)
- The use of an IV pole walker improves both patient and nurse satisfaction during early patient mobilization of post-surgical patients. (Nesbitt 2012)
PATIENT AWARENESS & EDUCATION
- The benefits of early mobility include better coordination and balance, as well as greater patient independence. (Morris 2010)
- When patients are informed about the benefits of early ambulation before undergoing surgery, patients become more proactive about seeking opportunities for early mobilization after surgery. (Kibler 2012)
STAFF EFFECIENCY
- Patients who have access to an ambulation platform have improved mobility outcomes and improved length of stay with fewer nurses and other staff required to implement ambulation. Nurses report that ambulation with an apparatus is easier for both staff and patients. (Henecke 2015)
- Nurses report that early mobilization improves patient independence and preserves patient dignity, which reduces the number of patient requests for assistance and decreases staff workload. (Hoyer 2015)
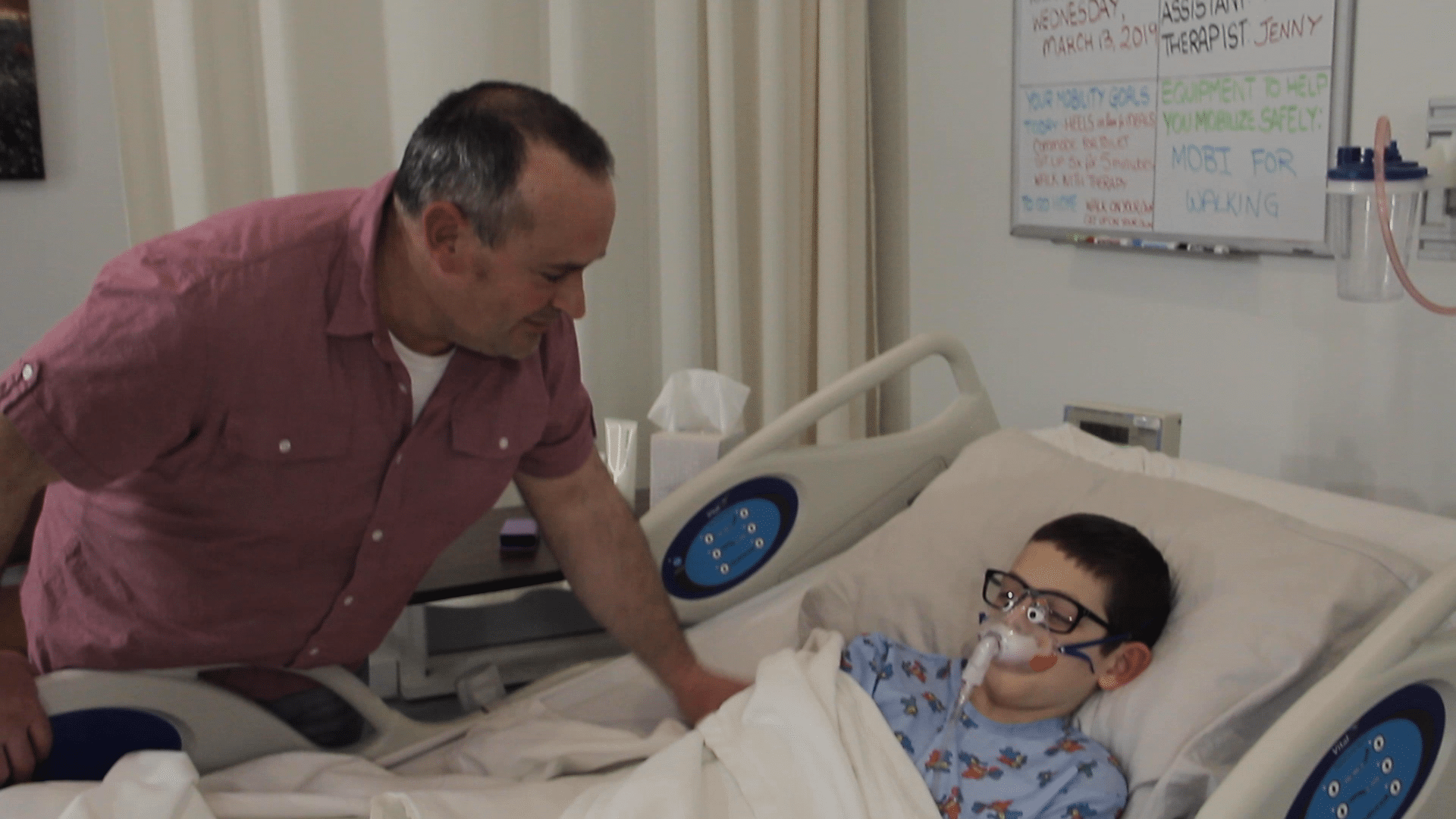
MOBILITY AS A HOSPITAL CULTURE
- Hospital-wide protocols and multidisciplinary teams dedicated to coordinating early mobility activities are important for improving ICU pediatric patient outcomes. (Piva 2019)
- Unit culture (established goals and protocols, coordinated effort) is a critical factor that determines whether nurses will implement patient mobility to the full extent of each nurse’s training and ability. (Krupp 2019)
- Incorporating early mobilization goals and achievements in electronic health records improves early mobilization coordination and improves early mobilization outcomes. The time required to achieve mobilization and the average length of stay decreased significantly, and the average patient ventilation time was decreased by 27 hours. (Anderson 2018)
Learn more about Livengood Medical Mobi Solutions.