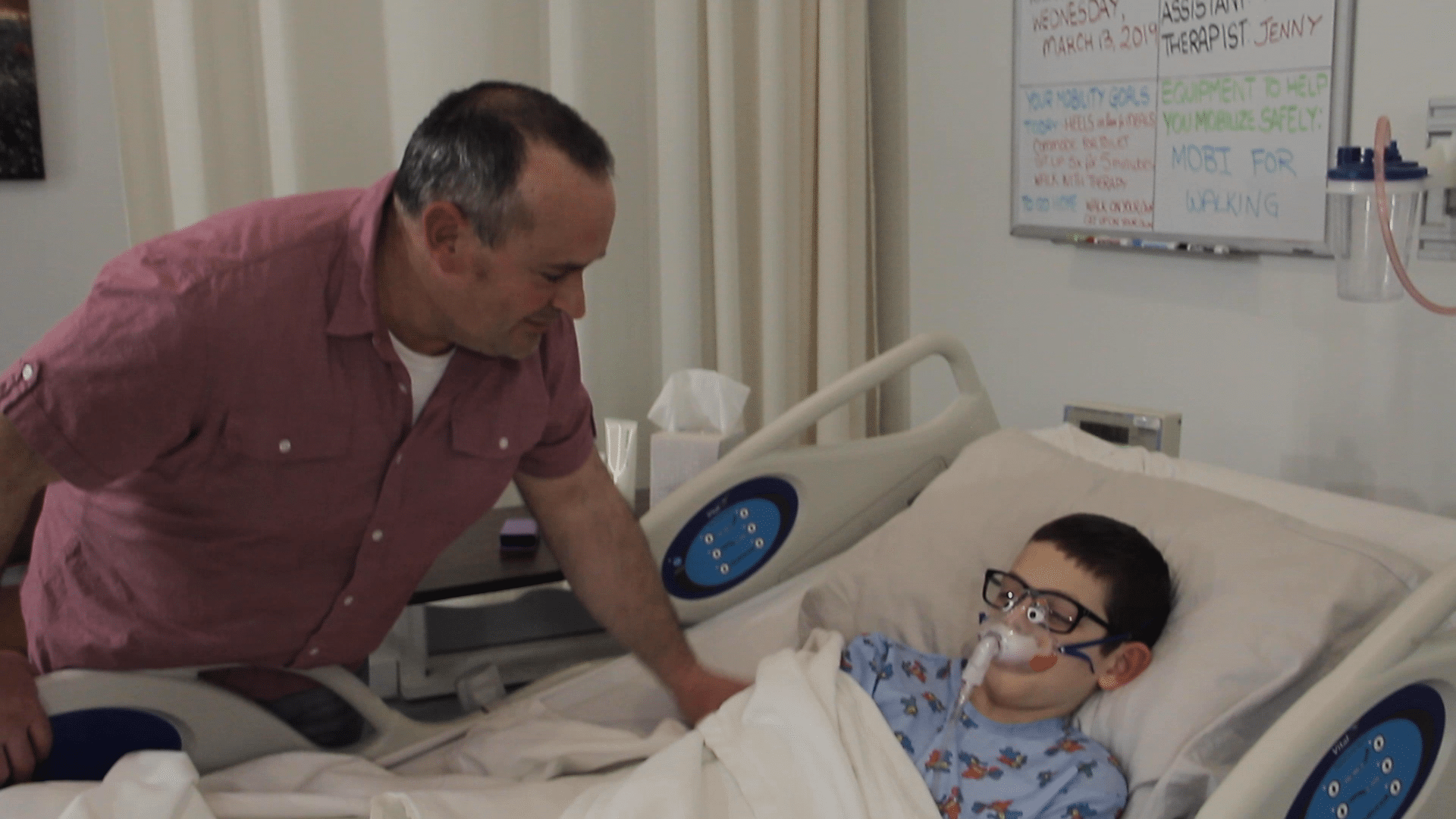
Patient Ambulation
Barriers to patient mobility. Most medical practitioners are keenly aware of the benefits of early mobility—it improves patient recovery times, lowers the risk of complications, and shortens overall length of stay. So why has it been so difficult to implement? Why have there been so many barriers to patient mobility? The most common barriers to patient mobility can be grouped in four categories: equipment, patient availability, staff availability, and unit planning.
Why Aren’t Patients Being Mobilized
Key Facts:
Barriers to patient mobility include:
EQUIPMENT
- In a survey of 500 U.S. ICUs, the number one listed barrier to early mobility was a lack of appropriate equipment. (Bakhru 2015)
- If key pieces of mobility equipment (mobility platforms, ceiling lifts, etc.) are not readily available, multiple assistants will be required to support the patient, and mobility may be deferred due to staff unavailability. (Krupp 2019)
PATIENT AVAILABILITY
- Patients who are called away for unscheduled procedures and tests aren’t present in the ward where nurses and physical therapists can implement early mobility.
STAFF AVAILABILITY
- Understaffing physical therapists decreases the frequency and length of early patient mobilization. (Johnson 2019)
- In an extensive study of community and academic hospitals, researchers determined that the greatest barrier to early patient mobility was the fear that “increasing mobilization of my inpatients will be more work for nurses.” Nurses directly reported that “they did not have enough time” to meet unit early mobilization goals (Hoyer 2015; Fontela 2018; Jolley 2014)
Learn more about Livengood Medical Mobi Solutions.